Calculation of the Premium Tax Credit
In 2014, a Supreme Court decision gave states the choice whether to expand Medicaid to cover adults with incomes below 138 percent of the poverty line. As a result, individuals earning between 100 and 138 percent of poverty can qualify for a premium tax credit in states that do not expand Medicaid, if states don’t already cover those individuals.
People can use their premium tax credit to buy four different types of plans offered through the marketplace in their state: bronze, silver, gold, and platinum. All plans sold in the marketplace must meet standards to ensure they provide adequate coverage. However, the plans vary, with bronze plans providing the least comprehensive coverage and platinum plans the most comprehensive.
Updated August 2024
As a result of the Affordable Care Act (ACA), millions of Americans are eligible for a premium tax credit that helps them pay for health coverage. The American Rescue Plan Act increased the size of the credits and made more people eligible for them beginning in the 2021 coverage year. The Inflation Reduction Act extended these enhancements through the end of the 2025 coverage year. This FAQ explains who is eligible for the tax credit, how the amount of an individual or family’s credit is calculated, how mid-year changes in income and household size affect tax credit eligibility, and how the reconciliation between the tax credit amount a person receives and the amount for which they were eligible will be handled.
Note that many guidelines and thresholds are indexed and change each enrollment year. For reference, please see the Yearly Income Guidelines and Thresholds Reference Guide.
The ACA created a federal tax credit that helps people purchase health insurance in ACA marketplaces (also known as exchanges). The “premium tax credit” is available immediately upon enrollment in an insurance plan so that families can receive help when they need it rather than having to wait until they file taxes. People can choose to have payments of the premium tax credit go directly to insurers to pay a share of their monthly health insurance premiums charged or wait until they file taxes to claim them.
The premium tax credit is available to individuals and families with incomes at or above the federal poverty level [1] who purchase coverage in the ACA marketplace in their state. Through the end of the 2025 coverage year, there is no maximum income limit for the premium tax credit. People whose benchmark premium costs more than 8.5% of household income qualify for a premium tax credit if they meet other eligibility criteria. A premium tax credit is also available to lawfully residing immigrants with incomes below the poverty line who are not eligible for Medicaid because of their immigration status.
To receive a premium tax credit, individuals must be U.S. citizens or lawfully present in the United States. They can’t receive a premium tax credit if they are eligible for other “minimum essential coverage,” which includes most other types of health insurance such as Medicare or Medicaid, or employer-sponsored coverage that is considered adequate and affordable.
In general, bronze plans require the most overall “cost sharing,” which means costs like deductibles and co-pays. Platinum plans would have the least overall cost sharing. For example, a bronze plan will likely have a higher deductible than a silver plan, while a platinum plan will likely have a lower deductible than a silver plan. People can purchase any of the four types of plans. But, cost-sharing reductions (which are available to people with incomes up to 250 percent of the poverty line) that lower deductibles and the total out-of-pocket costs under the plan, are only available to people who purchase a silver plan. (For more information on cost-sharing reductions, see Key Facts: Cost-Sharing Reductions)
ACA marketplaces also display catastrophic plans that are less comprehensive than bronze plans, but they are only available to people under the age of 30 and those who receive an ACA marketplace exemption due to hardship or lack of an affordable insurance option. A premium tax credit cannot be used to buy these plans.
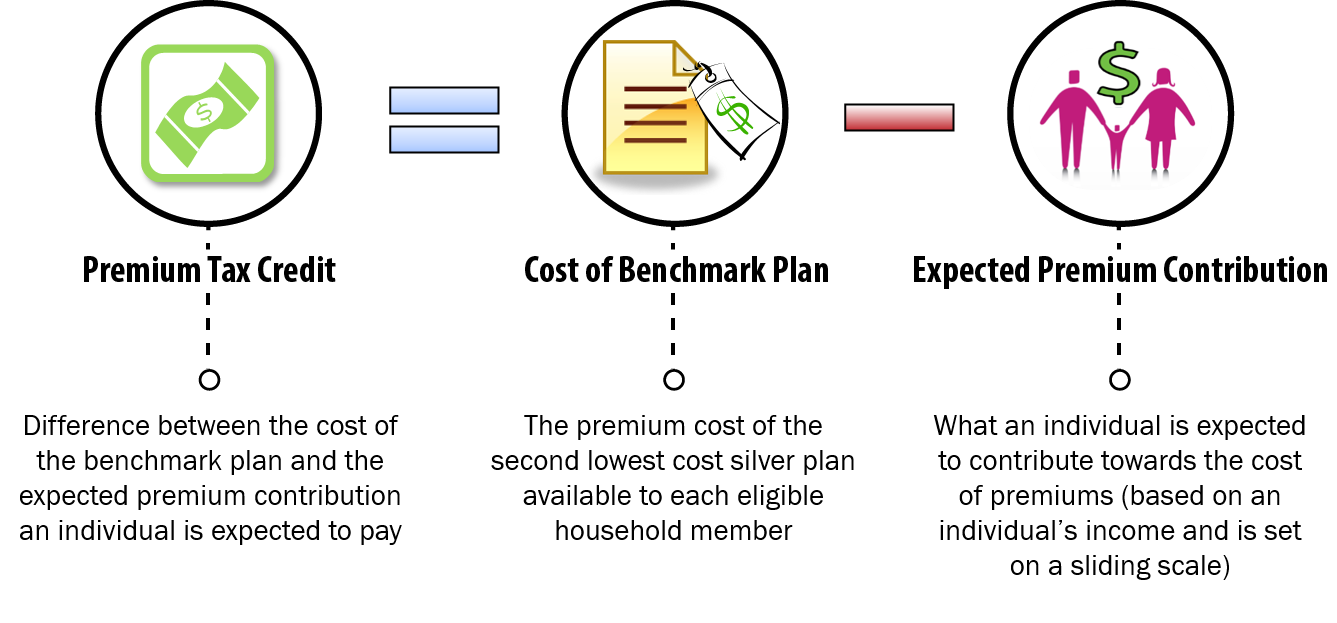
To calculate the premium tax credit, the ACA marketplace will start by identifying the second-lowest cost silver plan that that is available to each member of the household, called the “benchmark plan.” The amount of the credit is equal to the total cost of the benchmark plan (or plans) that would cover the family minus the individual or family’s expected contribution for coverage (see Figure 1).
| FIGURE 1: Calculation of the Premium Tax Credit |
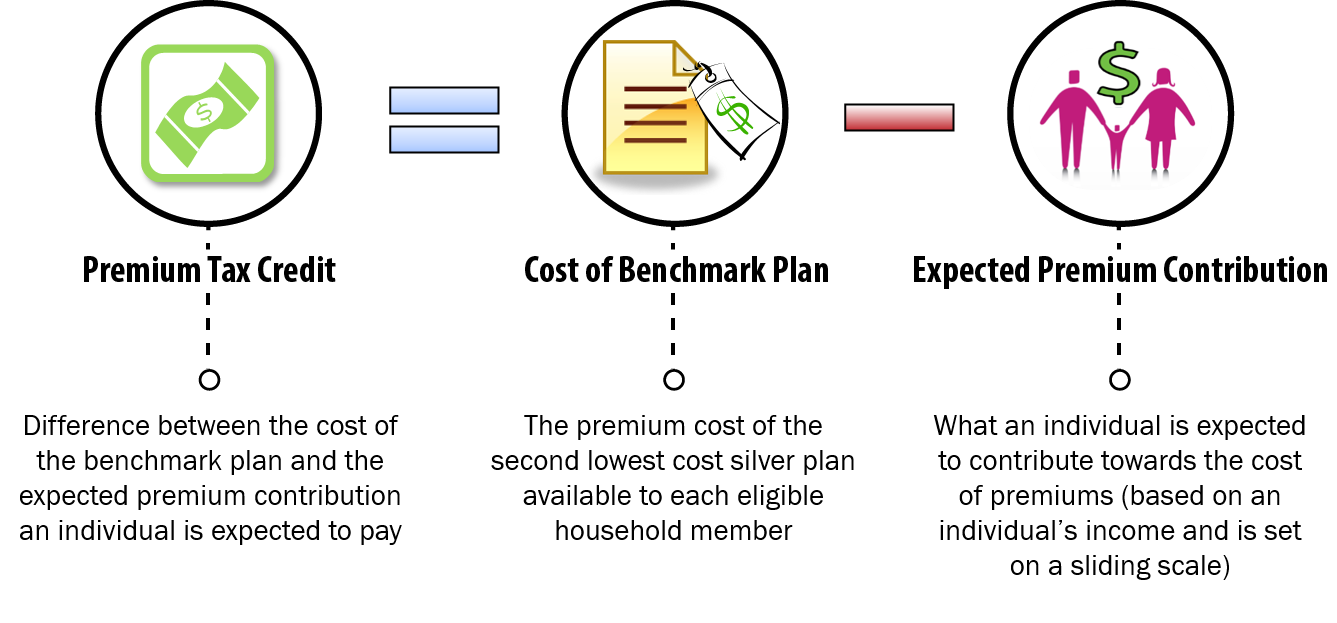 |
The individual or family is expected to contribute a share of their income toward the cost of coverage. That share is based on a sliding scale. Those who earn less have a smaller expected contribution than those who earn more, as shown in Table 1. For example:
| TABLE 1: Expected Premium Contributions at Different Income Levels (2024) | |||
| Income | Expected Premium Contribution Remaining After PTC | ||
| Percentage of poverty line | Annual dollar amount [1] | Premium contribution as % of income (in 2024) [2] | Monthly contribution |
| Family of four | |||
| $46,800 | 0% | $0 | |
| 200% | $62,400 | 2% | $104 |
| 250% | $78,000 | 4% | $260 |
| 300% | $93,600 | 6% | $468 |
| >400% | $124,800 | 8.5% | varies |
| Individual | |||
| $22,590 | 0% | $0 | |
| 200% | $30,120 | 2% | $50 |
| 250% | $37,650 | 4% | $126 |
| 300% | $45,180 | 6% | $226 |
| >400% | $60,240 | 8.5% | varies |
The benchmark plan is the second lowest-cost silver plan that is available to each member of the household. In many cases, such as for single individuals or for parents and their dependent children, coverage can be obtained through a single policy. In cases where there may not be a silver plan offered through the ACA marketplace that covers every single member of the household who is eligible for a premium credit (for example, because of the relationships of the individuals in the household), the benchmark may be based on the second lowest-cost silver option for the combined value of more than one policy.
The following example illustrates how the ACA marketplace would determine the applicable benchmark plan in some different situations:
The amount of the premium tax credit that an individual or family receives will take into account family size, geographic area, and age. For example, older people will get a larger premium credit than younger people, and an individual who lives in a high-cost state would receive a larger premium credit than an individual with the same characteristics who lives in a low-cost state. However, the premium tax credit will not cover the portion of the premium that is due to a tobacco surcharge. The following examples illustrate how age and tobacco use will affect the amount of the premium tax credit:
How much people will have to pay for coverage depends on the plan they choose. People can use the premium tax credit to buy a bronze, silver, gold, or platinum plan. The amount of the credit generally stays the same, regardless of which plan a person selects.
Gold and platinum plans will have higher premiums than the silver benchmark plan used to calculate the premium tax credit amount, so people will have to pay more than their expected contribution towards the premiums for these plans.
Bronze plans usually cost less than the benchmark plan. So, if an individual or family chooses a bronze plan, their share of the premium will be lower and possibly even zero. (The premium tax credit cannot exceed the plan premium,)
People must purchase a silver plan in order to get help with their cost-sharing expenses. So, purchasing a bronze plan may not be the lowest-cost option for an individual or family when all their out-of-pocket health care costs are considered.
Here’s how it would work, using the earlier example of John, a single individual:
People can apply through the ACA marketplace online, by mail, or in person. (The open enrollment period for coverage in 2025 is November 1, 2024 through January 15, 2025, and some states with State-Based Marketplaces have longer open enrollment periods.) Applicants need to provide information on their income, the people in their household, how they file their taxes, and whether they have an offer of health coverage through their job. Based on the information provided in the application, the ACA marketplace determines whether members of the household are eligible for a premium tax credit or other health care programs like Medicaid and the Children’s Health Insurance Program (CHIP).
No. People can choose to receive the credit in advance. Many people wouldn’t be able to afford the entire premium upfront and wait until they file taxes to get reimbursed. Getting the premium tax credit in advance allows them to pay their monthly insurance premiums and enroll in coverage purchased through the ACA marketplace. This is how it works:
People who receive advance payments of the premium tax credit will need to file taxes for the year in which they receive them. For example, someone who received advance payments of the credit for the 2024 calendar year will need to file a tax return and reconcile their APTC for 2024 before the April 2025 deadline.
Also, married couples who receive advance payments will need to file a joint return to qualify for the premium tax credit. There is an exception to this rule for survivors of domestic violence and individuals who have been abandoned by their spouses. In addition, an individual who is married but who qualifies to file taxes as Head of Household can also qualify for a premium tax credit.
A person who files taxes as Married Filing Separately cannot claim a premium tax credit unless they fall under one of two exceptions:
These exceptions can be claimed for no more than three consecutive years.
People who did not file a tax return in prior years can still qualify for a premium tax credit if they are otherwise eligible, but they will have to file a return for years they receive advance payments of the premium tax credit to qualify in future years.
No. Most people want to get the credit in advance because they can’t pay their entire monthly health insurance premiums without help, but if they choose, people can wait and receive the credit when they file their taxes.
People can also take a lower advance payment than the amount that is calculated based on their estimated income for the year and receive any remaining credit they are due at tax time.
The amount of the advance premium tax credit that people receive is based on a projection of the income the household expects for the year. The final amount of the credit is based on their actual income as reported on the tax return for the year the advance payment was received.
People who receive advance payments of the credit will have to reconcile the amount they received based on their estimated income with the amount that is determined based on their actual income as reported on their tax return. This means that people whose income for the year is higher than they previously estimated could have to pay back some or even all of the advance payments they received. On the other hand, people whose income ends up lower than estimated could get a refund when they file their taxes. For example:
One special rule is that if the advance payments received by people are greater than the final credit amount for which they are eligible, their repayment will be capped if their income is less than 400 percent of the poverty level. Table 2 shows the repayment limits. Note that if income for the year exceeds 400 percent of the poverty line, the individual or family would have to repay the entire amount of the advance payments they received.
| TABLE 2: Cap on the Amount of Advance Credits That Individuals and Families Must Pay Back (Tax Year 2024) [2] | ||
| Income as % of poverty line | Single taxpayers | Other taxpayers |
| Under 200% | $375 | $750 |
| At least 200% but less than 300% | $950 | $1,900 |
| At least 300% but less than 400% | $1,575 | $3,150 |
| 400% and above | Full amount | Full amount |
People who experience changes in income and household size over the course of the year should report these changes to the ACA marketplace when they happen because those changes can affect the amount of their premium tax credit. People whose incomes go down may be able to get a higher advance payment of the premium tax credit for the rest of the year, which would lower their monthly premium payments. (They also may receive more help with their cost sharing.) People whose incomes increase should report the change to have their credit for the rest of the year lowered and avoid having to pay back excess advance payments when they file their taxes. Household changes, which affect family income as a percent of the federal poverty level, such as having a baby or having a child leave the home, will also affect the amount of the credit and should be reported.
Another way people with fluctuating or unpredictable income can avoid having to pay back advance payments at tax time is to take less than the amount calculated based on their estimated income.
People who receive advance payments of the premium tax credit and who, partway through the year, receive an offer of employer coverage that is considered affordable and adequate should also report this change to the ACA marketplace, as should those who become eligible for other coverage, such as Medicare or Medicaid. Having other “minimum essential coverage” would make people ineligible for a premium credit for the rest of the year.
Yes. The premium tax credit is refundable, so people whose income taxes are lower than their premium tax credit can still take advantage of the credit. People eligible for the credit will be entitled to the full credit amount whether they take it in advance or wait until they file their taxes. For example:
[1] The marketplace uses the federal poverty guidelines available during open enrollment to determine premium tax credit amounts for the following year (e.g. 2024 guidelines for 2025 coverage).
[2] These percentages are indexed and will change each enrollment year. For yearly guidelines, see Reference Chart: Yearly Guidelines and Thresholds.